What Is the #1 Health Problem in the US?
 Oct, 28 2025
Oct, 28 2025
Heart Disease Risk Assessment Tool
Your Heart Health Assessment
This tool estimates your risk of developing heart disease based on key factors discussed in the article. Results are for informational purposes only and don't replace medical advice.
Heart disease is the #1 health problem in the US-and it’s been that way for over 80 years. Not cancer. Not diabetes. Not mental illness. Heart disease kills more people each year than all forms of cancer combined. In 2023, it took 702,000 American lives. That’s one person every 45 seconds. And the worst part? Most of these deaths are preventable.
It’s Not Just About the Heart
When people hear "heart disease," they think of heart attacks. But the term covers a whole group of conditions: coronary artery disease, heart failure, arrhythmias, valve problems, and high blood pressure. High blood pressure alone affects nearly half of all U.S. adults. And it doesn’t just strain the heart-it damages blood vessels, kidneys, and the brain over time.
What’s driving this? It’s not genetics alone. It’s not bad luck. It’s lifestyle-shaped by food, work, money, and environment. The average American eats 3,400 milligrams of sodium a day. The recommended limit? 2,300. Most people get more sugar in their morning coffee and cereal than in a candy bar. Fast food isn’t just convenient-it’s engineered to be addictive. And it’s everywhere.
The Obesity Connection
Over 42% of U.S. adults are obese. That’s more than 1 in 3. And obesity isn’t just a weight issue-it’s a metabolic disaster. It directly increases the risk of heart disease, type 2 diabetes, stroke, and certain cancers. The CDC says obesity-related medical costs hit $173 billion in 2019. By 2030, that number could double.
But here’s what most people don’t realize: obesity isn’t caused by laziness. It’s caused by systems. Low-income neighborhoods often have more fast-food outlets than grocery stores. Fresh produce is expensive. Public parks are scarce. Many people work two jobs and don’t have time to cook. A single parent working nights can’t easily find safe places to walk after work. When your body is constantly under stress-financial, emotional, physical-it starts storing fat as a survival mechanism.
Why the Medical System Isn’t Fixing It
The U.S. spends more on healthcare per person than any other country. Yet we rank 47th in life expectancy among developed nations. Why? Because our system rewards treatment over prevention. Doctors get paid to perform surgeries and prescribe pills-not to sit down and talk about diet, sleep, or stress.
Most primary care visits last 12 to 15 minutes. That’s not enough time to unpack years of unhealthy habits. And insurance often won’t cover nutrition counseling, gym memberships, or mental health support unless you’re already sick. Preventive care is treated like an optional add-on, not the foundation of health.
Meanwhile, pharmaceutical companies spend billions marketing drugs directly to consumers. Ads for cholesterol pills, blood pressure meds, and diabetes injections flood TV screens. They make you think the solution is a pill you can buy. But pills don’t fix broken food systems or stressful jobs. They just manage symptoms.
The Real Culprits: Food, Stress, and Inequality
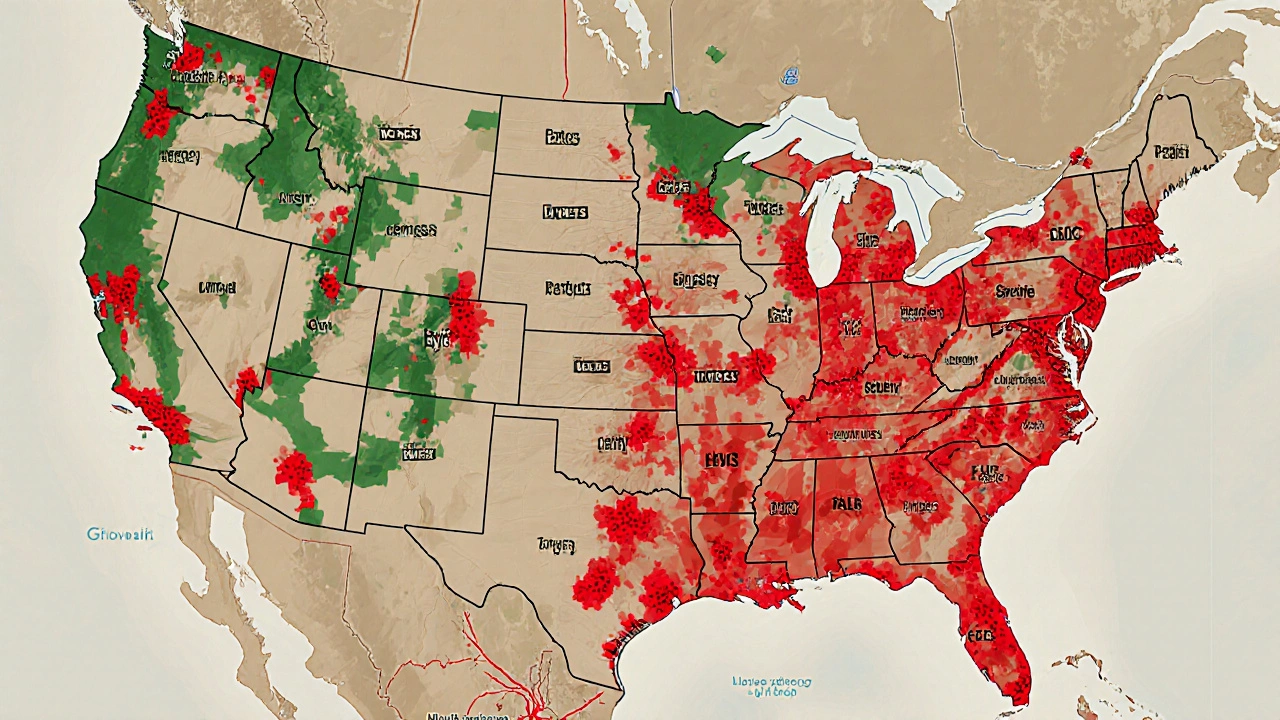
There’s a clear pattern: the worse your economic situation, the higher your risk of heart disease. People living below the poverty line are twice as likely to die from heart disease as those with higher incomes. Black Americans die from heart disease at higher rates than white Americans. Native American and Alaska Native populations face even higher risks.
Why? Because poverty isn’t just about money. It’s about access. Access to healthy food. Access to safe housing. Access to clean air. Access to time. People working multiple jobs don’t have time to exercise. People living near highways breathe polluted air that inflames arteries. People without health insurance skip check-ups until it’s too late.
Stress is another silent killer. Chronic stress raises cortisol, which increases blood pressure and fat storage. It also makes people crave sugar and fat. A 2024 study from Johns Hopkins found that people who reported high work stress were 40% more likely to develop heart disease-even after adjusting for smoking, diet, and exercise.
What Actually Works
There are proven solutions. But they don’t come in a pill bottle.
- Community gardens and subsidized produce programs have cut heart disease rates by 18% in pilot cities like Detroit and Philadelphia.
- Workplace wellness programs that include paid time for walking meetings and healthy meals reduced heart-related hospitalizations by 27% at a major Midwest manufacturer.
- City planning that prioritizes sidewalks, bike lanes, and parks led to a 15% drop in hypertension in Austin, Texas, over five years.
- Medicaid expansion in states that adopted it lowered heart disease death rates by 6% in just three years.
These aren’t fancy tech fixes. They’re basic human needs: access to food, safety, time, and care.

What You Can Do-Right Now
You don’t need to overhaul your life. Small changes add up.
- Swap one sugary drink a day for water or unsweetened tea. That alone can lower your risk of heart disease by 20% over five years.
- Walk for 20 minutes after dinner. No gym needed. Just move.
- Check your blood pressure once a year-even if you feel fine. High blood pressure has no symptoms.
- Ask your doctor for a lipid panel. Know your cholesterol numbers. Don’t wait until you’re in crisis.
- Support local food co-ops or farmers’ markets. Vote with your wallet.
And if you’re in a position to help others-whether you’re a teacher, employer, or community leader-push for policies that make healthy choices easier. Paid sick leave. Access to fresh food. Mental health coverage. These aren’t luxuries. They’re health interventions.
The Bottom Line
Heart disease isn’t inevitable. It’s a policy failure. It’s a food system failure. It’s a justice failure. We treat it like an individual problem when it’s really a collective one. The same systems that give us cheap, addictive food also give us poor health outcomes. The same systems that reward profit over people leave millions without the time or resources to stay healthy.
Fixing this won’t happen with better pills or more hospitals. It’ll happen when we start treating health like a right-not a reward for the rich, the lucky, or the disciplined. The #1 health problem in the U.S. isn’t a broken heart. It’s a broken system. And it’s time we fixed it.
Is heart disease really the biggest health problem in the U.S.?
Yes. Heart disease has been the leading cause of death in the U.S. since the 1920s. In 2023, it caused 702,000 deaths-more than cancer, accidents, and diabetes combined. It affects men and women of all ages, but risk rises sharply after 45 for men and 55 for women.
Can you prevent heart disease even if it runs in your family?
Absolutely. Genetics may raise your risk, but lifestyle choices control up to 80% of heart disease cases. Even people with a strong family history can reduce their risk significantly by eating whole foods, staying active, not smoking, and managing stress. A 2022 study in the Journal of the American College of Cardiology showed that healthy habits cut heart disease risk by 66% in high-risk groups.
Why isn’t the U.S. doing more to stop heart disease?
Because the system is built to treat illness, not prevent it. Insurance pays for surgeries and medications, not nutritionists or walking programs. Food companies profit from cheap, processed products. Politicians rarely face pressure to fix food deserts or workplace stress. Change requires shifting power and money away from profit-driven industries-and that’s harder than prescribing a pill.
What’s the link between obesity and heart disease?
Obesity doesn’t just add weight-it changes how your body works. Fat tissue releases inflammatory chemicals that damage blood vessels. It also raises blood pressure, triglycerides, and insulin resistance-all key drivers of heart disease. About 75% of people with heart disease are overweight or obese. Losing even 5-10% of body weight can dramatically improve heart health.
Are there any quick fixes for heart disease?
No. There are no shortcuts. Supplements, detox teas, or miracle diets won’t reverse heart disease. The only proven path is long-term lifestyle change: eating more vegetables and less processed food, moving daily, sleeping 7-8 hours, and managing stress. It’s not glamorous-but it’s the only thing that works.